Are you convinced that you’ve got a leaky gut? Just about every wellness website today talks about the dangers of leaky gut syndrome. And I’ll bet you’ve read how a leaky gut program will mend your belly.
Makes sense, yes?
The type of leaky gut program you’ll discover depends on who you listen to. Some suggest drinking bone broth all day while others recommend expensive supplement kits to solve your problem.
If you’ve been suffering a lot… and feel like the list of foods you can eat (without getting sick) is getting slimmer and slimmer, keep on reading.
Before you buy any leaky gut program, I’d like to share with you what I’ve learned from working with clients who tried many of these programs.
You deserve to know what may and may not work so that you don’t waste money (or time) on nothing more than false hope.
Are You Wondering — Is Leaky Gut Real?
I want to be straight with you here…
Leaky Gut Syndrome is NOT really a thing.
It’s a layman’s term to describe a very specific issue that’s better known in the medical world as “gut permeability.”
 Things like excessive stress, infections, food sensitivities, non-alcoholic fatty liver disease, and even chronic NSAID drug use can all be contributing factors.(1)
Things like excessive stress, infections, food sensitivities, non-alcoholic fatty liver disease, and even chronic NSAID drug use can all be contributing factors.(1)
(I specifically break down the problem with NSAIDs like ibruprofen here.)
Leaky gut as you know it affects your small intestine, in case you were wondering. Not the stomach or the colon… but specifically the small intestine where the large majority of nutrient absorption occurs.
You’ll likely get some pretty serious side-eye if you drop the phrase “leaky gut” in an exam room. Your doctor either won’t know what you mean or will go on the defense pointing out that leaky gut isn’t real.
While leaky gut syndrome isn’t the correct medical term, it certainly does describe a very real and often studied problem. For example, if you do a search of the term “gut permeability” on PubMed, you’ll discover over 3000 results matching your query.
And a variety of health concerns are linked, triggered, or exacerbated by gut permeability.
One paper published in February 2017 demonstrates the connection of leaky gut to painful migraines. The authors surmise through a literature review that improvements in gut flora could help reduce how often and how severe migraines would be with the help of appropriate probiotic supplementation.(2)
Breaking Down Leaky Gut Syndrome
 The term leaky gut is thrown around so much these day.
The term leaky gut is thrown around so much these day.
When I’ve pressed people to define or explain to me what leaky gut syndrome is, they struggle to answer. All they know is that they have it.
Every blog and functional practitioner talks about leaky gut.
Sensitive to gluten? You’ve got leaky gut. (Yes, you really do.)
Have celiac or an autoimmune disease? Yep, you’ve probably got it too.(3)
Knowing you have a leaky gut doesn’t mean you get what’s actually going on.
So allow me to break down leaky gut syndrome for you so that you actually get it!
From here on out, think of leaky gut like this —
Imagine a brick house. Focus your attention on one particular wall of brick and mortar.
A strong brick wall has the capacity to keep the house warm, dry, and bug-free. Much of this is due to the strength of the mortar mix between each brick.
Each brick of the wall represents a cell lining your gut. The mortar mix represents the seal filling the spaces (or tight junctions) between each cell (or brick).
I’m sure you can imagine why having a tight and leak-proof seal is important.
A tight seal means no leaky gut.
Then What Is Leaky Gut?
Since you now know that a tight seal of mortar between bricks prevents “leakiness”, then imagine what happens when the mortar is compromised.
Decay and crumbling allow little holes to form between the bricks. Bugs, ivy, and other invasive things that should stay on the outside of that wall find their way in.
Little holes become larger holes and with time, the brick wall is no longer sealed tight.
The same can be said of your small intestine when a state of leakiness or permeability arises.
Tight junctions between the cells aren’t so tight anymore. Now, partially undigested food proteins or microbial gut residents can take advantage of the gaps. This explains why chronic candida infections may be a trigger to developing celiac disease.(4)
Instead of staying inside the tube that is your small intestine, these intruders sneak beyond the gut wall to the inside of your body. These partially undigested food proteins can now trigger food sensitivities and immune system activation that can cause inflammation, potential autoimmunity, and a host of other issues.
This explains why you’ve noticed an increase in the number of foods that you’re sensitive to.
Or why you seem to get glutened from (what seems like) everything you eat.
Your diet becomes increasingly restrictive in an effort to try to avoid what are known as “trigger foods.”
Despite good intentions, this method of dealing with increased food sensitivities has been coined by some as the “disappearing iceberg diet.” Basically your “safe foods” become fewer, but you don’t necessarily feel any better.
Aside from the potential to end up with nutritional deficiencies because of such restrictive dieting, removing all these foods doesn’t address the root cause underlying leaky gut.
Nor will it likely allow the ongoing state of increase gut permeability to reverse enough so that you’ll start feeling better.
What Leaky Gut Is and What It Is Not
Functional medicine talks a lot about finding your root cause.
The truth is — leaky gut syndrome is not the root cause of why you’re sick. Merely “healing your leaky gut” may not get you back to feeling normal.
But, it is a necessary stepping stone that you cannot skip over on your health journey.
Leaky gut is not your end of the road… it’s just the beginning.
And it is a part of the ongoing problem that needs to be addressed no matter what else is wrong.

Solely taking out trigger foods from your diet will certainly help you feel better, but it can’t do the heavy lifting involved in resealing your gut.
You can’t drink bone broth all day assuming that your gut will heal. There are too many variables aside from what is listed in this article that make it difficult for bone broth alone to be as effective as you’re led to believe.
Keep in mind that the nutrient content within your bone broth can vary because of variations in cooking time or even the type of bones that are used.
There is also some legitimate concern about toxic heavy metals commonly stored in bone tissue that can end up in your bone broth.(5)
That’s why more is necessary to support gut tissue back towards a healthier state.
How Is Gluten Tied to Leaky Gut?
Gluten has an interesting relationship to leaky gut that we’re still learning about.
That said, the research is coming back saying that gluten’s got the magic touch.
No matter who eats it, the level of gut permeability is increased even if you’re not sensitive to gluten.
Take this groundbreaking research published in 2015 from a team that includes celiac pioneer Dr. Alessio Fasano who I’ve previously interviewed on my podcast.
They studied the level of gut permeability in four different groups: “celiac patients with active disease, celiac patients in remission, non-celiac patients with gluten sensitivity, and” people without celiac. In each group, a marked increase of gut permeability was noted, even in those who had no issue eating gluten due to gluten sensitivity or celiac disease.(6)
That’s why it is important to always exclude gluten 100% when doing a leaky gut program even if you don’t feel like you react to it.
Consuming gluten is completely counterproductive. Period.
And no, you can’t rely on gluten enzyme supplements to keep you safe when you eat out. I won’t go into the many issues with these products here since that’s a separate conversation for another time.
But I can share with you some tips on hidden gluten in restaurants so that you can avoid them.
#1 Reason Your Leaky Gut Program Isn’t Working
Your digestive system is pretty complex. Food has to go from whole food to smaller microscopic units in order to be absorbed in your gut. Each organ in your digestive tract serves a vital role.
If you’re missing certain factors at any point in the process of digestion, the burden is shifted downstream.
For example, if you don’t have enough stomach acid, proteins aren’t properly broken down. This issue is pretty common in people who complain about heartburn and GERD symptoms as well as in those with autoimmune diseases including celiac disease.(7)
There are three problems with having low stomach acid.
1. You’re more likely to develop Small Intestine Bacterial Overgrowth (SIBO).
2. These undigested proteins sneak into your body via the tight junctions (that are no longer tight) because you’ve got increased gut permeability. Your antibodies see them and think you’re being attacked… now you’ve got another food sensitivity and more inflammation.
3. Minerals critical to your health must be pulled away from proteins found in food. Low stomach acid (also more technically known as hypochlorhydria) can’t get the job done and so you can end up deficient in minerals as well as at greater risk for heavy metal toxicity.
But low stomach acid isn’t your only problem here.
There are necessary pancreatic enzymes and bile that are also needed.
Ultimately everything works together to ensure proper digestion and absorption. An issue with any one (or a combo) of missing factors presents an increased burden on your gut that slows the progress to heal leaky gut.
#2 Reason Your Leaky Gut Program Isn’t Working
Certain prescription as well as over-the-counter drugs can increase gut permeability.
The most notable group to cause leaky gut is called NSAIDs (non-steroidal anti-inflammatory drugs). I’ve written extensively about the issue HERE with these drugs as well as provided you a list of which drugs are considered to be NSAIDs.
 This is an important reminder as to why over-the-counter (OTC) drugs can have consequences and shouldn’t be taken as if there’s no risk or side effects possible.
This is an important reminder as to why over-the-counter (OTC) drugs can have consequences and shouldn’t be taken as if there’s no risk or side effects possible.
If you find yourself relying on NSAID medication, it’s time to get to the root behind what’s going on in the first place. That’s the most effective way to end your reliance on them.
And one other point – Alcohol is not your friend while doing a leaky gut program.
Another potential trigger for leaky gut is drinking alcohol. There is research to show that some develop an increase in gut permeability.
Consistent alcohol consumption can also throw your gut flora off balance leading to an increase in bacteria that isn’t helpful when you’re trying to reseal your gut.(8)
#3 Reason Your Leaky Gut Program Isn’t Working
Nutritional deficiencies can result when your gut’s been in a bad state for quite a long time. And as I mentioned above, if digestive factors aren’t up to par, then it increases the odds that you’ll have trouble absorbing the nutrients you eat.
Vitamins, minerals, amino acids, and other nutrients are important for healthy cells to be created in your body.
In fact, your small intestine will “turn over” every 3 to 5 days while your colon will do so every 5 to 7 days.(9)
While this doesn’t mean that you can heal leaky gut in less than a week, it does underscore the potential of healing when you provide your body with the right nutrition. And it’s even more important that you find out what nutrients you’re lacking so you can add to a proper diet and supplement regime.
#4 Reason Your Leaky Gut Program Isn’t Working
To put it bluntly, having unfriendly bugs in your gut has serious consequence.
They can wreak havoc on your digestion and increase the inflammation that you experience. Plus, their presence can perpetuate symptoms like chronic diarrhea, constipation, gas, and bloating.
Gut infections can be due to bacteria, parasites, or even fungus (like candida albicans). Heck, even SIBO which I mentioned above will make it really hard to start feeling better. And the waste products produced by these organisms only add to your digestive woes making you feel worse.
FYI — most of the leaky gut programs available for purchase online don’t address gut infections.
And if you don’t address the issue, then it’s not likely you’ll feel better.
This is one of the biggest reasons why my clients have come to work with me after doing two or three different DIY programs they’ve purchased. Because they never had guidance through the process, their gut infections were never identified or addressed. As a result, the symptoms didn’t improve no matter how long they kept trying to heal their gut.
It’s upsetting to realize the money and time that’s literally been wasted.
And it’s an utter shame to discover that you’ve been spinning your wheels using generic supplement kits that aren’t intended for people who’ve got a complicated gut situation going on.
Talk about frustrating!
That’s why it is important to work with a practitioner who knows what signs to look for that indicate a problem.
Additionally, certain functional testing can be helpful to identify issues that don’t show up on a conventional stool panel. Tests such as the Organix Comprehensive Profile (a urine test) and the GI Effects Gastrointestinal Function Comprehensive Profile (a stool panel) offer a different perspective that often provide insight we can work with.
#5 Reason Your Leaky Gut Program Isn’t Working
Hidden trigger foods can be a huge problem. A lot of people assume that only more common foods like gluten, dairy, or eggs are a problem. But that’s not entirely true.
One of the hallmarks of leaky gut syndrome is that you can have sensitivities to other foods you’d never suspect like strawberries, lettuce, or asparagus. It might surprise you to find out that a really healthy food could be problematic.
But when the floodgates of the gut are open, developing sensitivities to other foods you eat is fair game.
 If you just take gluten (and the other big foods out) as recommended by general leaky gut program kits, you may be unintentionally irritating your gut over and over with hidden trigger foods.
If you just take gluten (and the other big foods out) as recommended by general leaky gut program kits, you may be unintentionally irritating your gut over and over with hidden trigger foods.
That’s why it’s best to figure out what foods are causing moderate to severe reactions and work to remove them during your leaky gut program.
Doing so can dramatically reduce the inflammatory response that’s often seen in those with leaky gut syndrome.
In my own case, I was sensitive to more than just gluten. The list included eggs (both the yolk and white), casein, cashews, pistachios, mangos, and the entire cruciferous family of vegetables.
I honestly had no idea how sick all of these foods made me.
After maintaining a diet free of them for 3 months, I had lost close to 20 lbs of inflammation in my body. You can see in this picture of me how inflamed my face was months before I got so sick that I couldn’t wake up in the morning even after 11 hours of sleep.
#6 Reason Your Leaky Gut Program Isn’t Working
Unaddressed chronic stress has a huge impact on your gut. Stress plays a role in immune system responses as well as the integrity of the mucosal lining of your digestive tract.
Too much stress for too long of a period of time beats up your gut.
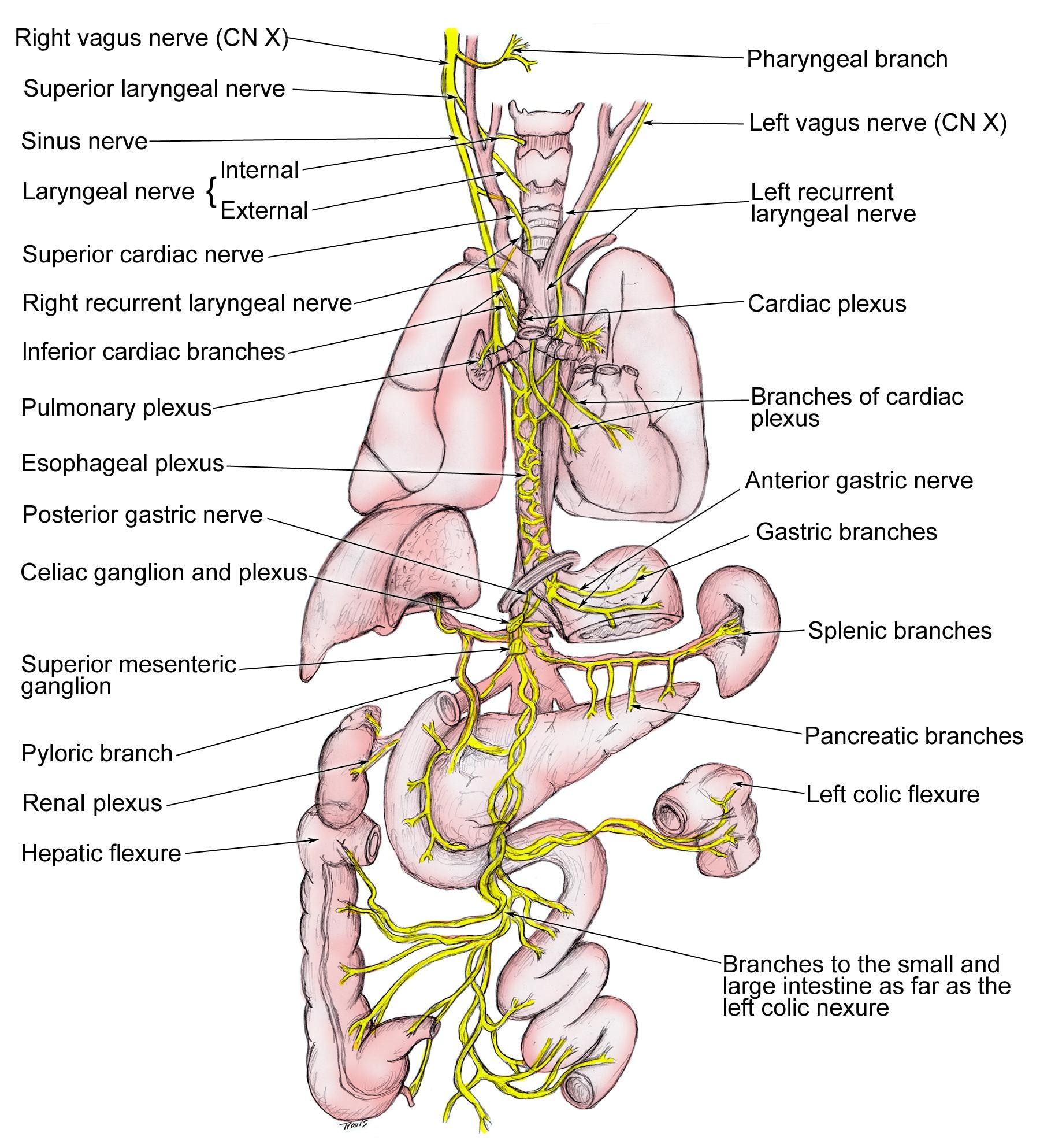
While you might dismiss mental stress directly impacts your gut, know that the vagus nerve connects the two. This is why the gut is often called your second brain.
In this lovely diagram highlighted in yellow, the vagus nerve is the longest cranial nerve in your body wandering extensively through many organs.
The vagus nerve gets its name from the word “vagabond” and connects to the GI tract via the gut-brain axis as well as through the hypothalamic-pituitary-adrenal (HPA) axis. You may have heard of the HPA axis before since HPA axis dysregulation is the medical term for adrenal fatigue.(10)
That’s why stress in your mind can be felt through your digestive tract as well as why stress within the digestive tract can impact your mind.
Unfortunately, addressing chronic stress is one of the necessary steps that people never want to take. I can’t tell you how many excuses I’ve heard about why month after month someone can’t find time to do a simple breathing exercise for 2 minutes.
I get it… solutions that are “free” don’t seem like they’d have any value or benefit.
These exercises or practices aren’t a priority because you don’t necessarily see the vast impact immediately. And it’s also incredibly easy to say “I’ll do it later” and never actually get to it.
But, avoiding or minimizing the power of mindfulness and stress reduction is like shooting yourself in the foot.
Buying a kit of supplements will never replace stress management. You can take those supplements for years, but if you don’t address stress effectively, you may not see the results you were hoping for.
#7 Reason Your Leaky Gut Program Isn’t Working
It’s entirely possible that what looks like a leaky gut cure isn’t what it’s cracked up to be. One of the biggest reasons why a standard one-size-fits all leaky gut program won’t work is because it’s not a specific enough fit for you.
As a general protocol, DIY leaky gut protocol kits cover the bare minimum to address leaky gut assuming there are no other reasons continuing to aggravate your digestive tract.
But since you’ve read this far, you know that there are six reasons why a general leaky gut program may not work for you. No matter the number of testimonials it has, you’ve no clue of how sick those individuals were before they began as well as how their health situation compares to your own.
Everyone is different.
You are unique both in who you are as well as how you ended up sick.
And it’s important to keep that in mind.
Any combo of the six reasons I just shared means that you’re more likely to need a customized leaky gut program. Otherwise, you’ll likely feel that no matter what you do, you just can’t heal your gut.
Two or three different programs later, you may then come to this exact conclusion and find yourself seeking out a customized solution.
I hope you don’t wait that long as many of my clients have. It adds up to a lot of lost time, money, and energy trying to fix something that needs a different, unique approach.
What Type Of Leaky Gut Program Actually Works
Because so much about you is unique — your genes, your day-to-day, your diet, your stressors, etc. — so too does your journey back to better health (and a resealed gut) require a unique plan.
The reasons you have leaky gut may be entirely different from why I (or anyone else you know) developed it.
And if you don’t feel like the cookie cutter approach often used by conventional medicine has been helpful, then the chances of a generic supplement kit solving your problems are pretty slim.
Yes, some people do get better using them. But most people don’t (even after using two or three different programs).
Diet changes may need to be made, but as I said — gluten will definitely have to go. Here’s a sample of what clients who work with me can expect if they’re just avoiding gluten.
Work With An Experienced Gut Expert (Who’s Been In Your Shoes)
You’re not “just another patient.”
Your concerns are a big deal to you because they impact even the smallest things in your life.
They can make all the difference between having a productive, great day or barely treading water through one that’s a total disaster.
I know how this feels because I was ignored by doctors for months being told that I was fine. Though I felt horrible, my symptoms didn’t seems to matter even if I couldn’t wake up after 11 hours of sleep to get to work on time.
It wasn’t until someone listened to me that I actually got answers that made a difference.
And that is key… to find someone who gets what you’re going through, believes your inner knowing that something is wrong, and is willing to put what seem like unlikely clues together.
To create an effective plan to heal leaky gut must include sifting through more of your health history than anyone has in the past.
It’s not uncommon that pieces of “your story” that have been blown off by your doctor are relevant. I’ve found through my training and clinical nutrition practice that they’re often critical clues. And they need to be framed around appropriate labs and patterns that help us uncover the root cause.
(Psst… you don’t always need to do every test if your practitioner asks good questions and can make sense of a lot of information.)
From there, the results need to be practically tailored to meet you where you are so that you can actually implement steps that get results.
If you’re in need of gut support, I invite you to take a moment to learn about how I work with clients as their nutrition co-pilot. It’s my mission as a clinical nutritionist to provide you with tools and support so you can resolve ongoing IBS and leaky gut issues and get back to feeling better than you have in a long time.
REFERENCES:
1. Miele L, Valenza V, La Torre G, Montalto M, Cammarota G, Ricci R, Mascianà R, Forgione A, Gabrieli ML, Perotti G, Vecchio FM, Rapaccini G, Gasbarrini G, Day CP, Grieco A. Increased intestinal permeability and tight junction alterations in nonalcoholic fatty liver disease. Hepatology. 2009 Jun;49(6):1877-87.
2. Dai YJ, Wang HY, Wang XJ, Kaye AD, Sun YH. Potential Beneficial Effects of Probiotics on Human Migraine Headache: A Literature Review. Pain Physician. 2017 Feb;20(2):E251-E255.
3. Rallabhandi P. Gluten and celiac disease–an immunological perspective. J AOAC Int. 2012 Mar-Apr;95(2):349-55.
4. Corouge M, Loridant S, Fradin C, Salleron J, Damiens S, Moragues MD, Souplet V, Jouault T, Robert R, Dubucquoi S, Sendid B, Colombel JF, Poulain D. Humoral immunity links Candida albicans infection and celiac disease. PLoS One. 2015 Mar 20;10(3):e0121776.
5. Monro JA, Leon R, Puri BK. The risk of lead contamination in bone broth diets. Med Hypotheses. 2013 Apr;80(4):389-90.
6. Hollon J, Leonard Puppa E, Greenwald B, Goldberg E, Guerrerio A, Fasano A. Effect of Gliadin on Permeability of Intestinal Biopsy Explants from Celiac Disease Patients and Patients with Non-Celiac Gluten Sensitivity. Nutrients. 2015;7(3):1565-1576.
7. Miceli E, Lenti MV, Padula D, Luinetti O, Vattiato C, Monti CM, Di Stefano M, Corazza GR. Common features of patients with autoimmune atrophic gastritis. Clin Gastroenterol Hepatol. 2012 Jul;10(7):812-4.
8. Leclercq S, Matamoros S, Cani PD, Neyrinck AM, Jamar F, Stärkel P, Windey K, Tremaroli V, Bäckhed F, Verbeke K, de Timary P, Delzenne NM. Intestinal permeability, gut-bacterial dysbiosis, and behavioral markers of alcohol-dependence severity. PNAS. 2014;111,42:E4485-E4493.
9. Barker N. Adult intestinal stem cells: critical drivers of epithelial homeostasis and regeneration, Figure 1: Epithelial self-renewal in the intestinal epithelium. Nature Reviews Molecular Cell Biology. 2014;15,19–33
10. de Jonge, WJ. The Gut’s Little Brain in Control of Intestinal Immunity. ISRN Gastroenterology. Volume 2013 (2013), Article ID 630159, 17 pages.